Hi all,
Over the years there’s been a proliferation of demographic-related archetypes created using the EHR RM and intended to be used for clinical recording purposes and explicitly designed with a simple, light touch that is adequate for recording in a consult note, a referral or an extract to send to a new GP practice.
We often get pushback from the engineers because it means we don’t end up using proper Master Patient Indexes or Healthcare Provider Indexes etc. So, just to be clear, I’m not talking about the creation of an intraEHR address book either - it is never, or should never be, the intention to add the names or contact details so that it could be updated over time etc. That should clearly be done in a way that is sustainable and separate from the EHR.
Think of these examples:
- the name and contact details for a lawyer who holds a physical copy of an advanced care record;
- the name and contact details of a carer in a referral;
- the name, role and contact details of a member of a care team;
- the role and contact details of a named primary contact person within an organisation;
- details about a relative in a family history record; or
- a witness to an epileptic fit; and
- the location of a fall or accident.
With that view in mind, and in the context of a multitude of divergent models in various CKMs, we want to try to consolidate and converge back to a common, shared pattern.
Today I’ve sent out 3 CLUSTER archetypes for review - Person, Organisation and Address.
There are additional archetypes for Structured name and Structured address that can be reviewed as fast followers, but act to extend each of these archetypes.
The archetypes are based on:
- current Australian standards AS 4846-2006 Health Care Provider Identification & AS 5017-2006 Health Care Client Identification. Standards Australia.
- current FHIR resources, although there are a couple of tweaks but still mappable; and
- an outdated version of ISO/TS 22220:2007 Health informatics — Identification of subjects of health care.
If anyone can check them against the latest ISO versions that would be much appreciated as I don’t have access to a copy. 
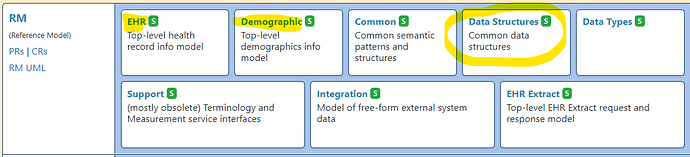
We have the intent to revise the demographics archetypes built on the Demographic RM at some point in the future - we are certainly intending for them to be compatible.
Examples of template containing the 3 core archetypes can be viewed here:
Please adopt the archetypes if you’d like to participate in the review process
Regards
Heather