CONTEXT:
We use the openEHR-INSTRUCTION.medication_order.v3 that is packed inside the COMPOSITION.request.v1. The design came up during coaching sessions as well as how the current EHR handles such orders. After having written my assignment for IREB Requirements Modeling I concluded, that there might be better approaches how to handle the inpatient’s medication orders during a “normal” hospitalization.
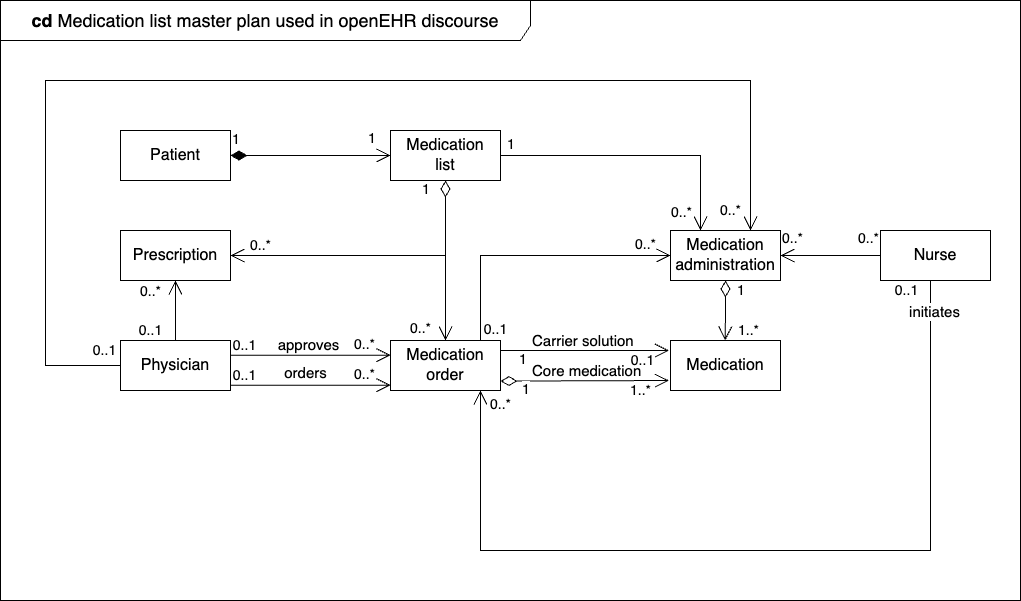
Consequently, I am planning to remodel the whole thing to fulfill the following requirements summarized and heavily simplified in the following class diagram:
3 QUESTIONS:
- Do you store medication orders redundantly in openEHR such that the same instance is listed in the medication list, the medication order request (use case description as in FHIR), in the prescription and so forth?
- Or do you manage any medication instruction (order, requests, prescriptions and so forth) in one composition, namely in COMPOSITION.medication_list.v1 (which I will do)?
- May a patient have several medication lists in openEHR?