I’m not so sure that this example is a good clinical requirement on which to propose possible RM changes.
-
Recording an actual body weight at a point in time is one clinical concept.
-
Recording a change in body weight over an interval, as an actual in ‘kg’ or as ‘%’ is a semantically separate concept. And if we record as % we need to ensure a clear linkage back to the original weight that the weight loss is relative to?
While we can technically apply RM/tooling acrobatics to record the delta using the ‘Weight’ measurement using the ‘Change’ attribute over an unspecified interval of time in a single archetype, it doesn’t mean that we should do so. I’ve always struggled with Sam’s initial modelling of this in the original body weight archetype, going way back to 2004. It’s a neat little package in theory but I’m concerned about:
- mixing ‘close, close but different’ semantics in one archetype.
- how we implementers communicate to implementers that Actual weight is associated with a Point in time event and ‘Change’ is the diff between two actual weights at points in time with the change period defined as an interval (or is it a point in time recording linking to the two existing OBSERVATIONs.
In fact I’m of the opinion that actual weight and the change in weight should be recorded as two discrete clinical concepts in two separate archetypes.
The commonest and cleanest clinical scenario is to record separate weights accumulating over time, maybe even graphed. No brainer, modelled well in the existing OBSERVATION.
Recording the diff is more complex as we don’t often record it as an independent measurement. Why?
- Because the diff is relative and only relevant when knowing both the current and previous actual measurements. We need a clear reason to calculate it, much less record it, because it may be quite a different calculation yesterday or tomorrow.
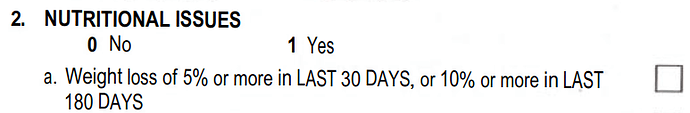
- In my experience, most often the calculation is triggered within the context of screening for cancer or debility/frailty in aged care or similar, most often needing to answer a questionnaire’s question like 'has the patient lost >5k or 10% of their body weight in the ’ - Answer is Yes/No.
For example:
If the delta is recorded, as it may well be on occasion or to provide the evidence for a Yes/No questionnaire answer, it is still only a delta that is only meaningful at the time of recording (ie as a point in time delta, but relating to original measurements at two discrete points in time that may be (correctly or incorrectly) expressed/interpreted as an interval of ‘last 30 days’ or ‘last 6 months’. It assumes that you have today’s weight and the weight exactly 30 days or 6 months ago. And we usually only have approximations or guesses of the previous weight.
It is messy.
H